Many doctors are unwilling to prescribe traditional sleeping tablets because of concerns that they can lead to addiction and tolerance. GPs often turn to other types of drugs that display sedative side effects and instead prescribe these to help people sleep.
These drugs are used ‘off label’: they’re not licensed to treat certain conditions but can be effective, nevertheless. Quetiapine is one such off label drug used to treat insomnia. You can find more information about quetiapine from NICE on their website.

Quetiapine is an antipsychotic medication
In the UK quetiapine is licensed for the following indications:
- schizophrenia
- treatment of mania in bipolar disorder
- treatment of depression in bipolar disorder
- prevention of mania and depression in bipolar disorder
- in addition to primary medication to treat major depression.
In the USA quetiapine is commonly sold under the brand name Seroquel.
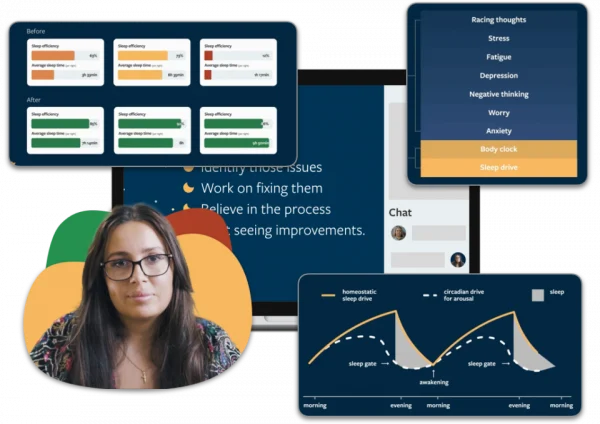
Sleep better without quetiapine
People who have sleeping problems often turn to quetiapine, hoping for a quick fix. Most people don’t realise that there are more effective ways to treat your sleeping issues without side effects. With Sleepstation you can significantly improve your sleep without relying on medication. Sleepstation will help you:
- fall asleep quickly
- get all the sleep you need
- spend less time awake in bed
- wake feeling refreshed.
Sleep better without quetiapine
Get support from sleep experts, plus self-help tools.
Working with an expert who really grasps your situation is key to unlocking real sleep, effortless sleep. You deserve to sleep well and to work with people who have the right knowledge and expertise to help you get there.
Begin your journey to a lifetime of better sleep with:
- a full week of unlimited access to our highly-trained sleep coaches.
- direct contact and professional advice, with no waiting lists.
- expert insights to control and repair your sleep.
- lifetime access to an ever-growing library of sleep tools and resources.
Quetiapine as a treatment for primary insomnia
Despite a lack of evidence pointing to its effectiveness in helping improve sleep, quetiapine is increasingly prescribed at low doses to manage sleep disorders.
For instance, between 2005 and 2012, prescriptions of quetiapine for sleep disturbances increased by 300% in Canada.1
In addition, data from a wide-ranging US survey found that between 1999 and 2010, quetiapine was the fourth most common drug prescribed for insomnia (11%).2
Neither of these countries had approved the drug as a licensed alternative to treating insomnia.3
Is quetiapine useful as a treatment for insomnia?
Quetiapine can improve symptoms that may interfere with sleep, such as reducing feelings of anxiety and depression. So it’s difficult to evaluate its effects as a sleep medication when the drug is designed to improve symptoms that, in themselves, also affect sleep.
To establish whether the drug has a direct effect on sleep, we can look at trials with healthy volunteers who do not show any signs of psychiatric illness. These studies allow the drug’s influence on sleep to be accurately assessed.
However, where quetiapine is concerned, there have been very few studies that have evaluated its effect on sleep in patients who were not also experiencing a psychiatric illness.
One study evaluated 14 healthy males who were given placebo or quetiapine at 25mg and 100mg doses for three consecutive nights.4
Both doses of quetiapine produced statistically significant improvements in objective and subjective ratings of sleep including:
- total sleep time
- sleep efficiency
- sleep latency
- duration of stage N2 sleep.
Despite these positive effects, the 100mg dose was found to decrease the amount of REM sleep, which is a stage of sleep important for our emotional wellbeing.
The 100mg dose also increased the number of periodic leg movements and two subjects taking quetiapine experienced orthostatic hypotension, which is a drop in blood pressure when a person moves from sitting to standing.
In a study of people with primary insomnia, 25 participants received either 25mg of quetiapine or a placebo. No significant improvements were seen in how long people slept for, how quickly they fell asleep, their daytime alertness or sleep satisfaction.5
A more recent study replicated insomnia by using traffic noise to keep people awake. They found that 50mg quetiapine increased sleep continuity and total sleep time when compared to placebo.
However, there was evidence of hangover effects in the morning with quetiapine causing daytime sleepiness and difficulty concentrating.6
How quetiapine could disrupt your sleep
Quetiapine has a long list of side effects and a large number of these are potentially disruptive to your sleep. It’s hardly ideal for a drug that’s meant to help you sleep!
Side effects that could disrupt your sleep — and that occur in at least one in 10 people taking quetiapine — include:
- dizziness, weakness and shortness of breath
- feeling sleepy
- headaches, fever, shortness of breath
- a dry mouth
- weight gain and increased appetite
- a rapid or irregular heartbeat
- constipation, upset stomach, indigestion, vomiting
- swelling of arms or legs
- sleep disorders
- feeling irritated
- thoughts of suicide.
In the clinical trials of quetiapine there have been other reports of side effects that could potentially disturb sleep.
Two patients, on low dose quetiapine for insomnia, discontinued the drug due to akathisia — a movement disorder characterised by a feeling of inner restlessness and an inability to stay still.7
In another study of low dose quetiapine for insomnia in people diagnosed with Parkinson’s disease, two out of 13 participants stopped using the drug due to an exacerbation of restless leg symptoms.8

Quetiapine or sleeping tablets?
One of the most cited reasons for avoiding the use of using traditional sleeping tablets to treat insomnia is a concern that they’re addictive. This is why GPs look to prescribe alternatives that are not associated with addiction.
However repeated studies have shown that quetiapine has abuse potential. 910111213 This raises serious questions concerning its suitability as a replacement for either benzodiazepines or so-called ‘Z’ drugs.
Does the evidence warrant use of quetiapine for insomnia?
While there’s some evidence that quetiapine can improve sleep in healthy participants, only minor improvements in sleep are seen in patients with insomnia.
The unclear results seen in the few trials described above provide little evidence to justify prescribing quetiapine for insomnia. 121314 The general consensus amongst studies is that quetiapine should be avoided as a drug for insomnia.
The results are reinforced by a review of quetiapine for use in insomnia which concluded that any benefit in the treatment of insomnia has not been proven to outweigh potential risks. 15
This is true even in patients who require treatment for a condition for which quetiapine is approved, such as schizophrenia.
The general consensus amongst studies is that quetiapine should be not be used as a drug for insomnia.
So it’s difficult to understand how a drug hardly renowned for improving insomnia — and associated with such a broad range of side-effects and a potential for addiction and abuse — can be so widely prescribed.

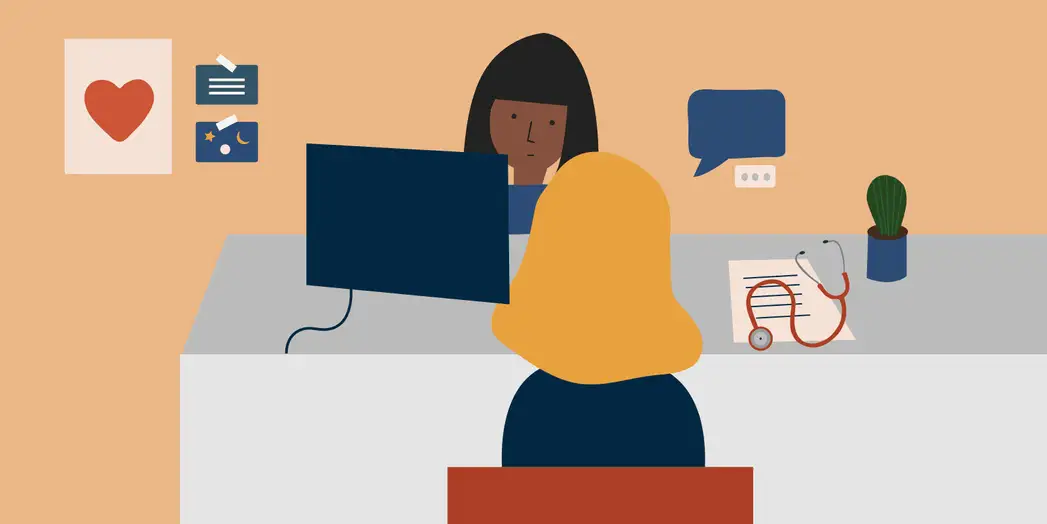
Should you question quetiapine?
If you’re prescribed quetiapine by your GP or psychiatrist then you have a legitimate case for asking why they’re using this drug rather than the benzodiazepines and the ‘Z’ drugs that have proven effectiveness in the treatment of insomnia.
Remember this is about your health and your sleep, not theirs. You have every right to discuss the most appropriate treatment for your condition.
Sleepstation offers a highly effective, drug-free approach to treating insomnia
The best starting point for treating insomnia that has lasted for more than four weeks (chronic insomnia) is well-recogised to be cognitive behavioural therapy for insomnia (CBTi).
Unlike sleeping pills, CBTi helps you overcome the underlying causes of your sleep problems rather than just alleviating the symptoms. We’ve been using this type of therapy in our online sleep clinic for well over a decade, and it’s incredibly effective.
The first step in treating insomnia with CBTi is to identify the causes of the insomnia. At Sleepstation, we guide you through this, then help you to address the causes of your sleep problem and provide you with the tools you need to rebuild your sleep.
With help from our sleep experts, therapists and experienced sleep coaches who’ll support you at every step, you’ll better understand your sleep and learn ways to combat your sleep problems and stop them reoccuring. Most people see an improvement their sleep after just three sessions.
Sleepstation’s programme works if you’re currently taking sleeping tablets and can help to reduce the amount you’re taking, or stop altogether. You can get started in just a couple of clicks, here.
Summary
- Quetiapine is neither approved nor recommended for primary insomnia although the drug is often prescribed off-label as a sleep aid.
- There is evidence of addiction to quetiapine.
- Side effects associated with quetiapine — such as next morning hangover symptoms and daytime fatigue — means that patients should be cautious.
- Drugs such as quetiapine cannot treat a sleep problem, they will only mask them.
- Sleepstation is a clinically-validated, drug-free alternative that is proven to improve sleep.
References
- Pringsheim T, Gardner DM. Dispensed prescriptions for quetiapine and other second-generation antipsychotics in Canada from 2005 to 2012: a descriptive study. CMAJ Open 2014;2:E225-32. ↩︎
- Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999-2010. Sleep 2014;37:343–9. ↩︎
- Marston L, Nazareth I, Petersen I, Walters K, Osborn DPJ. Prescribing of antipsychotics in UK primary care: a cohort study. BMJ Open 2014;4:e006135. ↩︎
- Cohrs S, Rodenbeck A, Guan Z, Pohlmann K, Jordan W, Meier A, et al. Sleep-promoting properties of quetiapine in healthy subjects. Psychopharmacology (Berl) 2004;174:421–9. ↩︎
- Tassniyom K, Paholpak S, Tassniyom S, Kiewyoo J. Quetiapine for primary insomnia: a double blind, randomized controlled trial. J Med Assoc Thai 2010;93:729–34.Cohrs S, Rodenbeck A, Guan Z, Pohlmann K, Jordan W, Meier A, et al. Sleep-promoting properties of quetiapine in healthy subjects. Psychopharmacology (Berl) 2004;174:421–9. ↩︎
- Karsten J, Hagenauw LA, Kamphuis J, Lancel M. Low doses of mirtazapine or quetiapine for transient insomnia: A randomised, double-blind, cross-over, placebo-controlled trial. J Psychopharmacol 2017;31:327–37. ↩︎
- Catalano G, Grace JW, Catalano MC, Morales MJ, Cruse LM. Acute akathisia associated with quetiapine use. Psychosomatics 2005;46:291–301. ↩︎
- Juri C, Chaná P, Tapia J, Kunstmann C, Parrao T. Quetiapine for insomnia in Parkinson disease: Results from an open-label trial. Clin Neuropharmacol 2005;28:185–7. ↩︎
- Waters BM, Joshi KG. Intravenous quetiapine-cocaine use (“Q-ball”). Am J Psychiatry 2007;164:173–4. ↩︎
- Hussain MZ, Waheed W, Hussain S. Intravenous quetiapine abuse. Am J Psychiatry 2005;162:1755–6. ↩︎
- Pinta ER, Taylor RE. Quetiapine addiction? Am J Psychiatry 2007;164:174–5. ↩︎
- Pierre JM, Shnayder I, Wirshing DA, Wirshing WC. Intranasal quetiapine abuse. Am J Psychiatry 2004;161:1718. ↩︎
- Erdoğan S. Quetiapine in substance use disorders, abuse and dependence possibility: a review. Turk Psikiyatri Derg 2010;21:167–75. ↩︎
- Wine JN, Sanda C, Caballero J. Effects of quetiapine on sleep in nonpsychiatric and psychiatric conditions. Ann Pharmacother 2009;43:707–13. ↩︎
- Pigeon WR. Diagnosis, prevalence, pathways, consequences & treatment of insomnia. Indian J Med Res 2010;131:321–32. ↩︎