The menopause is a time of huge hormonal upheaval in a woman’s body, so it’s not surprising that the process can have a big impact on your sleep. In fact, sleep disorders are recognised as one of the most widely reported problems associated with the menopause.
Each woman will experience the menopause differently. Some may breeze through it with barely a symptom but up to 50% of women report problems that can interfere with their daily life and nightly sleep.
In this article, we’ll explain exactly what’s going on in the body that can cause sleep problems around the menopause. We’ll also look at what steps you can take to improve your sleep as you approach, go through and come out of this transition.
What exactly is the menopause?
Most of us know that women of a certain age will go through the menopause but specifically what this process entails might not be so clear. In the simplest terms, the menopause is the stage of life when a woman’s periods stop and her reproductive years end.
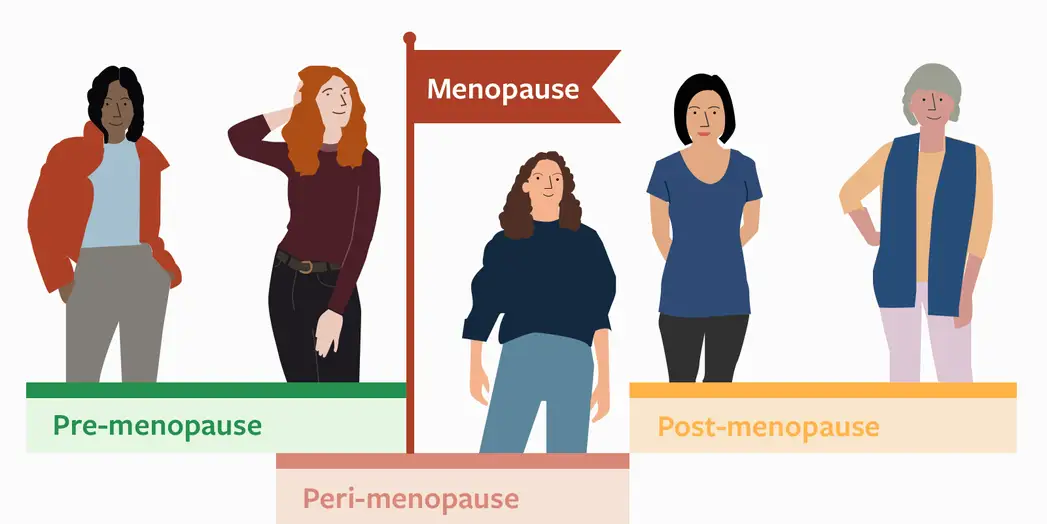
Before menopause (pre-menopause) a woman generally has regular periods and her hormones rise and fall in set rhythms, which can cause sleep quantity and quality to dip and rise each month.
With the approach of the menopause, these rhythms begin to lose their regularity and hormone levels can change both erratically and dramatically. Sleep then often begins to suffer.
Menopause can occur naturally or artificially. In the latter case, it’s brought about for a medical reason — often following the surgical removal of the ovaries or as a result of chemotherapy or radiation therapy.
When menopause is brought about artificially, symptoms can be more intense and they tend to begin more abruptly than during natural menopause. In this case their treatment will differ slightly and can be longer than for natural menopause.
Natural menopause is not a short or simple transition. It occurs gradually over several years and can be thought of as having defined stages1 which can be split up into three main periods of time, based on how hormone levels are changing in the body.
1. Peri-menopause
- Usually begins when a woman is in her 40s.
- Periods become irregular.
- Oestrogen levels become erratic, whilst slowly decreasing.
- Progesterone levels decrease.
- Sleep disturbances can start to become more noticeable.
2. Menopause
- Usually occurs when a woman is in her 50s.
- Is reached when a woman has had no period for 12 consecutive months.
- Oestrogen levels decrease dramatically.
- Progesterone levels decrease.
- Sleep disturbances may become sleep problems.
3. Post-menopause
- The stage of life following menopause.
- Periods no longer occur.
- Oestrogen levels remain permanently low.
- Progesterone levels remain permanently low.
- Sleep is generally lighter and more easily disturbed.
It’s the changes in hormone levels (particularly oestrogen and progesterone) which are behind most of the sleep problems that arise during the menopause.
Behind the scenes of the menopause: the hormones at play
There are myriad hormones that change across the menopause but the main players involved in sleep disturbances are generally accepted to be oestrogen, progesterone, cortisol and melatonin.
We’ll look at what each does and how it can contribute to sleep problems during the menopause.
Firstly oestrogen, as it’s the one most people think of in relation to female health. This hormone is generally considered responsible for hot flushes but oestrogen has a huge range of effects in the body, not least when it comes to sleep.
Oestrogen, at appropriate levels, can:
- Increase REM sleep, which is important for memory, mood and learning
- Decrease the time it takes to get to sleep (sleep latency)
- Decrease the number of awakenings after sleep occurs
- Increase total sleep time
- Help in regulating body temperature during sleep
- Regulate neurotransmitters such as serotonin that are important for controlling mood.2
So, when oestrogen levels begin to dip during the menopause, it’s easy to see from the list above how it could have knock-on effects on various aspects of your sleep.
Next is progesterone which, though not as well-known as oestrogen, also has roles to play in sleep. This hormone is known to have a sedative effect, so can help to make you feel sleepy. It also stimulates respiration, so helps with breathing while you’re asleep.
When progesterone levels start to decline during the menopause, sleep quality can also decline and breathing problems during sleep can become more pronounced. We’ll look at this in more detail further along.
Thirdly, there are changes to melatonin levels during the menopause. Commonly thought of as the sleep hormone, levels of melatonin decrease gradually with age but are known to decrease significantly during the menopause.3 For more information see our article on melatonin.
Finally, cortisol is a hormone often known as the ‘fight or flight’ or stress hormone, as it’s one of our brain’s signals of danger. When we experience something scary, stressful or dangerous, our cortisol levels increase and we feel anxious or stressed.
During menopause, levels of cortisol have been shown to be elevated at night-time, which can lead to increased feelings of stress and anxiety. Additionally, cortisol levels spike just after a hot flush, which can leave a woman feeling ‘on alert’ during the night and can make it difficult to fall back asleep.
As mentioned earlier, there are many other hormonal changes going on during the menopausal transition — and considerable interplay between them — so it’s no wonder it can feel overwhelming to experience.
It’s reassuring to know that research is constantly improving our understanding of how hormone levels alter during menopause. The knock-on effect of this is that new ways and potential treatments to improve sleep during this transition are also regularly being discovered.
Also discussed earlier, changes in the levels of many of these hormones start to occur a long time before the menopause itself and the effects on sleep can initially be subtle. We’ll now look more closely at how sleep can begin to be compromised as a woman heads towards the menopause.

Peri-menopause: setting the stage for sleep problems
For many women, the seed is often sown for developing sleep problems way before the menopause itself. The years leading up to the menopause are frequently the busiest of our lives: it’s a time when career, family and life in general are often rather hectic.
So it’s no wonder that with action-packed lives, sleep regularly suffers during this period. Minor sleep issues that a woman experiences during this time have the potential to slowly snowball, going from mild sleep disturbances to moderate problems and eventually resulting in a full-blown sleep disorder such as insomnia.
The peri-menopause lasts, on average, around four years. For some women this stage is over in a few months and for others it may take as long as a decade. During this time, levels of the main sex hormones — progesterone, oestrogen and testosterone — all begin to decline.
But levels can also rise and fall erratically. Oestrogen levels, in particular, can change dramatically and deviate far from their pre-menopause patterns. It’s these ups and downs that are responsible for hot flushes, palpitations and sweats, which are known collectively as vasomotor symptoms.
When a person is experiencing these symptoms at night, it’s hardly surprising that their sleep will suffer. Sleep becomes disrupted and both the quality and quantity of sleep a woman achieves can be jeopardised.
In fact, pre-menopausal sleep problems are a significant predictor of menopausal sleep problems1 so if you’re already experiencing poor sleep before the menopause, you’re at higher risk of having sleep issues during the menopause.
This is why it’s always a good idea to give yourself a ‘sleep MOT’. Ask yourself:
- Am I getting enough sleep for my needs?
- Do I feel recharged in the mornings, or ready to crawl back into bed?
- Do I frequently need to catch up on sleep?
- Could I improve my bedtime routine?
The articles section of the Sleepstation website has a wealth of reading material on how to improve your sleep, so it’s an excellent first step and a brilliant resource of expert advice and information on how to make sure you’re getting a good night’s sleep.
We’ve established that women in the peri-menopausal period can often be unwittingly setting themselves up for developing more serious sleep problems. In women transitioning through the menopause, self-reported rates of ‘sleep difficulties’ are somewhere between 40-56%4 and figures from America’s National Sleep Foundation put this at more than 60%.
But it’s not just hot flushes and night sweats that are to blame for menopausal sleep problems. Women also report higher rates of restless legs syndrome (RLS), sleep apnoea and insomnia. Stress, anxiety and depression are all also reported to increase during this time and all can contribute to menopausal sleep problems too.
It’s time to take a more detailed look at these contributing factors and find out how you can minimise their impact on your sleep. There are so many ways that the menopause can affect your sleep that it often feels like you’re fighting a losing battle. But don’t despair! There are a wealth of treatments available to help you tackle the menopause — and its impact on your sleep — with confidence.
Symptoms of menopause

Vasomotor Symptoms (hot flushes and night sweats)
Hot flushes are thought to occur in 60-80% of women during the menopausal transition5 6 and they’re probably the symptom that most of us associate with the menopause. As mentioned earlier, they’re largely thought to be due to hormonal changes.
Hot flushes cause a sensation of heat in the upper body. Usually, the face, neck and head are involved and the person may feel hot and sweaty while also having palpitations and flushing. These symptoms can cause feelings of anxiousness and can result in chills, in addition to feeling hot.
For some, they can occur as frequently as every hour and for others as infrequently as once per week/fortnight.7 Independent of frequency, many women report their sleep being disturbed due to night-time awakenings from hot flushes.
While we know a lot about this symptom, it might be surprising to learn that we don’t fully understand what causes hot flushes and how exactly they disturb sleep. Yes, they are caused by hormonal changes but it’s not as simple (as is often stated) to say that oestrogen is wholly to blame.
In fact, sleep disturbance due to hot flushes is much more complex than this. How they affect sleep is also still under study. There are two main ways that these episodes are studied and the first is subjective: the person experiencing the hot flush records when and how frequently they occur during sleep.
Secondly, they can be measured during a sleep study. This is known as polysomnography and involves readings being taken from sensors placed on the body while you sleep. Usually, these measure heart rate, blood oxygen level, brain activity, body and eye movement during sleep.
When self-reporting and polysomnography are taken together, something interesting is seen: not all hot flushes wake the person from sleep. Self-reporting can under-record how many flushes are actually occurring during the night and therefore not all of them will disturb sleep.
Women report that their sleep is disturbed by hot flushes but studies have actually pointed to the arousal from sleep occurring both before or after the flush. What is clear, however, is that hot flushes are strongly associated with disturbed sleep.
Several hypotheses have been put forward as to why they disturb sleep. Changes to blood pressure, heart rate and core body temperature have all been examined and shown to occur around hot flushes.8
Regardless of what exactly wakes you with a hot flush, what is important to note is that when sleep is disturbed by this symptom, the person tends not to just have a brief arousal but a full awakening.
Once awake, the time to fall back asleep can be anything from a couple of minutes to more than an hour. When this pattern repeats night after night, this sleep disturbance can easily lead to insomnia.
So what can be done to improve your sleep when it’s being disturbed by hot flushes and night sweats?
Firstly, it’s a good idea to look at your sleeping environment to ensure it’s not contributing to the problem.
Your bedroom should be on the cooler side rather than toasty. A general guideline is to keep the temperature around 18°C.
As your bedding is going to contribute to how hot you get during the night, one useful way to control the temperature is to have multiple layers of bedding. That way, if you get too hot, you can just remove a cover and hopefully get back to sleep easily.
For excellent advice and information on how temperature contributes to good sleep, you can read our article on temperature and sleep.

Finally, what you wear to bed can help to regulate your body temperature. Avoid man-made materials such as polyester as these can trap heat and sweat close to you. Cotton or linen nightwear can help to dissipate heat away from the body.
Take note of what you’re eating and drinking too. Caffeine and alcohol are no friends to good sleep at the best of times and both may exacerbate feelings of hot flushes. Additionally, avoiding spicy food may work for some women.
Healthy lifestyle choices such as maintaining a healthy weight, taking regular exercise and trying to quit nicotine can help to improve your sleep.
Hormone therapies include oestrogen therapy and progesterone/progestin therapy can improve sleep quality in women experiencing hot flushes.4 5 Both hormones can be given together or separately to improve sleep.
If you still feel that your hot flushes are interfering with your sleep, there are several other medications that your doctor can prescribe. These can help reduce the severity of your hot flushes.
Menopause and sleep apnoea
Sleep apnoea is a sleep disorder in which your breathing stops and starts during sleep. The most common type of sleep apnoea is obstructive sleep apnoea (OSA), which occurs when muscles in the back of the throat relax too much and obstruct the airflow and normal breathing.
It can disturb sleep by rousing the person after a bout of not breathing but often these periods of rousing do not lead to full awakenings. Sometimes this can happen many times over the course of a night and in severe cases there can be hundreds of episodes in just one period of sleep.
Often, the person experiencing OSA will not even know that something is happening with their breathing during the night but might:
- feel excessively tired the next day
- wake with headaches
- have low mood and feel irritable.
Other times, the episodes may fully awaken the person, who may have sensations of choking, gasping for air or snorting. When the person is fully roused from sleep in this way, it can make it harder for them to fall back asleep.
How does this relate to the menopause? Quite surprisingly, around 20% of women are estimated to experience sleep apnoea during the menopause.9 The incidence of OSA is known to increase in peri-menopause and during the transition through the menopause,10 peaking in post-menopause.
Once again, the cause of this increased incidence is thought to be down to hormonal changes. It’s believed that progesterone is particularly important for the good functioning of upper airway muscles. When the muscles relax too much, breathing can be obstructed and OSA can result.
In women going through the menopause, progesterone levels being to dip, so muscle tone in the upper airway can be reduced.11 Studies have shown that this effect can be reversed when progesterone is administered to women.
There’s also data to suggest that oestrogen — or a combination of oestrogen and progesterone — can improve symptoms of sleep apnoea in menopausal women too.4
Additionally, weight gain and obesity are huge risk factors for OSA. The menopause is known to be associated with weight gain and an overall redistribution of body fat, with more fat being stored in the throat area. This, in turn, puts additional pressure on the muscles keeping the airway open.
The general risk of developing OSA increases with age and is also known to increase with poor sleep12, so trying to improve your sleep habits may improve symptoms of sleep apnoea.
For people with mild sleep apnoea, it’s also a good idea to try to lose any excess weight. Regular exercise encourages better sleep, so by exercising you can enjoy the multiple benefits of increasing fitness, helping control weight, reducing apnoea and improving your sleep.
When OSA is more severe, there are other treatment options available, such as wearing a specially fitted mouthpiece while sleeping. These hold the mouth/jaw/tongue in a specific manner to aid breathing.
Another option is a continuous positive airway pressure (CPAP) machine, which involves wearing a face mask attached to a machine to provide constant air pressure which keeps the airways open while you sleep.
Menopause and restless leg syndrome
Restless leg syndrome is a condition that causes a severe urge to move the legs and can be accompanied by unusual, unpleasant or tingling sensations in the legs. It’s not clear exactly what causes RLS, but there are several underlying conditions that may trigger it.
Many women report experiencing RLS during the menopause but this is one symptom that is linked to but not caused by the menopause. What we know is that RLS is twice as prevalent in women compared to men and that the incidence of RLS increases with age.
This may be why women report RLS more often during the menopausal transition. It’s thought that falling oestrogen levels could play a role in RLS during the menopause. Oestrogen is important for muscle relaxation, so the changes that occur in oestrogen levels during this transition could contribute to RLS symptoms.12
If you think you’re experiencing RLS then speak to your healthcare provider as it’s a sleep problem that responds very well to treatment.
Happily, there are various options available to treat it. Methods include:
- non-drug treatments such as massage or exercise
- reducing caffeine intake
- using distraction techniques in bed
- medication to control the movement and calm the muscles.
Menopause and depression, anxiety and stress
Adequate, good quality sleep plays a huge role in regulating our moods. Given that the menopause has the potential to disrupt sleep in a whole manner of ways, it’s not surprising that this lack of sleep can cause symptoms of depression, anxiety and stress to worsen.
Conversely, depression and mood disorders can all cause us to lose sleep. It’s well-established that depression and insomnia go hand-in-hand. People with depression have higher rates of insomnia and people with insomnia are more likely to be depressed. For greater insight into this, see our article on sleep and depression.
Whether menopause causes depression itself is still the subject of much debate13 but many studies note increases in depressive symptoms around this transition. For example, one study found the greatest levels of depression in women between the ages of 45-55, which fits well with this period of hormonal upheaval.14
The menopause brings with it its own stresses and strains. It can feel like there’s no end to the hot flushes, cold sweats, hormonal and bodily changes over which you have no control. So it’s no shock that people going through the menopausal transition report higher levels of anxiety and stress.

While we know that insomnia and depression are linked to each other, when deciding which one came first it can be a bit of a chicken and egg scenario. But when considering how insomnia can lead to depression during the menopause, it can be useful to think of it as a cascade effect.
1: Symptoms such hot flushes, restless legs and anxiety lead to disturbed sleep.
2: Disturbed sleep becomes more persistent and regular.
3: The disturbed sleep becomes severe enough to be classed as insomnia.
4: Persistent insomnia leads to depression.
If you’re experiencing changes in mood that you think are down to poor sleep or are interfering with your sleep, Sleepstation can help. We combine psychology and sleep science with dedicated support to improve sleep. By addressing your sleep problem, you will likely see an improvement in your mood. And when you sleep well, you feel better.
Menopause and insomnia
Given that the menopause can affect your sleep in myriad different ways, it’s no surprise that insomnia is the most widely-reported sleep disturbance associated with it.
Insomnia can be defined as occurring when you have persistent difficulty getting to sleep or staying asleep. It can be acute or chronic: when the frequency is at least three times per week for at least three months, it’s classed as chronic insomnia.
Insomnia brings with it daytime symptoms that impair your ability to go about your daily life. You may:
- feel daytime sleepiness
- have poor focus
- struggle to get tasks done
- experience a dip in mood
- become more irritable.
During the menopausal transition, women commonly report sleep disturbances but putting a figure on how many experience actual insomnia proves more difficult. One study found 26% of the peri-menopausal women they recruited were experiencing insomnia disorder.14

Another study puts the figure between 31% and 42% for peri-menopausal women showing symptoms of insomnia. Interestingly, this study also found that women in the later stages of peri-menopause had the greatest levels of insomnia symptoms.15
When self-reported insomnia was further examined by a sleep study, results showed that 50% of the women involved were sleeping fewer than six hours a day, indicating that they were experiencing a significant sleep deficit.14
Studies have also shown that there is a significant correlation between experiencing hot flushes and developing insomnia in the peri-menopause.
What all of these studies lead us to is the finding that levels of insomnia in menopausal women are higher than in the general population. So what is being done to help women sleep well during the menopause?
Thankfully, there is plenty of research into improving sleep during this transition and many treatment options are available.
Treating sleep disorders during the menopause
Treatment options for hot flushes, restless legs and sleep apnoea will all differ in their approaches and have been discussed in each section above. Sometimes, however, a combination of disorders can respond to a single treatment.
For example, hormone therapy can improve perceived sleep quality in women experiencing both hot flushes and sleep apnoea and low dose antidepressants can reduce symptoms of both hot flushes and RLS.
When it comes to treating insomnia during the menopause, many options have been examined, including:
- low dose antidepressants
- hormone therapy
- yoga
- dietary supplementation
- exercise
- cognitive behavioural therapy for insomnia (CBTi).416
While there are benefits to each treatment trialled, CBTi is considered the primary intervention for insomnia during the menopause.17
CBTi is both medication-free and extremely effective. It centres around examining the sleep habits, thought patterns and behaviours of a person in order to identify what’s coming between them and sleep.
By getting to the root of the sleep disorder in this way, CBTi then helps the person to build healthy sleep habits and remove negative behaviours that may be interfering with their sleep.
In the context of insomnia during the menopause, numerous clinical trials have shown that CBTi is the most effective treatment for insomnia during the menopause.14 16 17 18
There’s additional research showing that CBTi improves sleep in women experiencing hot flushes, sleep apnoea and RLS18 19 20 21 22 so the benefits of CBTi for women during the menopausal transition are multiple.
While the menopause can affect your sleep, you don’t need to feel like it’s something that just has to run its course. Sleep issues that arise during the menopause can progress to sleep disorders that remain in the post-menopausal years, too.
CBTi is the approach we use at Sleepstation so we know just how effective this type of treatment can be. We’ve used CBTi to successfully resolve sleep problems for thousands of men and women across all ages and from diverse backgrounds.
So whether you’re approaching the menopause, going through it or have come out the other side — and feel like your sleep problems are affecting your daily life — we can help. We have decades of expertise in sleep science and have helped many thousands of people to sleep well through our digitally delivered sleep improvement programme.

Summary: How can I sleep better during menopause?
While the menopausal transition can affect sleep, there’s no reason to let it disrupt your sleep or to think it’s something you can’t change. Here’s our list of some simple steps you can take to ensure you get a good night’s sleep:
- Keep your bedroom cool and well-ventilated
- Try having layers of bedding so that you can easily adjust the heat
- Sleep in loose clothing — cotton and linen are usually best
- Avoid spicy food, especially near bedtime
- Cut back on nicotine, coffee and alcohol if possible
- Limit screen-time in the evening
- Establish and maintain a bedtime routine
- Exercise regularly each day, but not too close to bedtime
- Look at ways to manage your stress and try to make time to relax.
These tips are general ways to improve sleep during the menopause but if you have a sleep disorder, you may need more a tailored solution. That’s where Sleepstation’s NHS-accredited sleep improvement programme can help.
If you are going through the menopause and feel like your sleep is suffering, sign up to Sleepstation. Whether you’re struggling with hot flushes, restless legs, insomnia or just feel like you’re always waking up tired and can’t figure out why, we’ll help you find your way to back to good sleep.
References
- Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging: Addressing the unfinished agenda of staging reproductive aging. Menopause. 2012;19(4):387–95. ↩︎
- Eichling PS, Sahni J. Menopause related sleep disorders. J Clin Sleep Med. 2005;1(3):291–300. ↩︎
- Jehan S, Jean-Louis G, Zizi F, Auguste E, Pandi-Perumal SR, Gupta R, et al. Sleep, melatonin, and the menopausal transition: What are the links? Sleep Sci. 2017; 10(1):11-18. ↩︎
- Baker FC, de Zambotti M, Colrain IM, Bei B. Sleep problems during the menopausal transition: prevalence, impact, and management challenges. Nat Sci Sleep. 2018;10:73–95. ↩︎
- Joffe H, Massler A, Sharkey KM. Evaluation and management of sleep disturbance during the menopause transition. Semin Reprod Med. 2010;28(5):404–21. ↩︎
- Kronenberg F. Menopausal hot flashes: a review of physiology and biosociocultural perspective on methods of assessment. J Nutr. 2010;140(7):1380S-5S. ↩︎
- Freedman RR, Roehrs TA. Lack of sleep disturbance from menopausal hot flashes. Obstet Gynecol Surv. 2005;60(2):106–7. ↩︎
- Baker FC, Forouzanfar M, Goldstone A, Claudatos SA, Javitz H, Trinder J, et al. Changes in heart rate and blood pressure during nocturnal hot flashes associated with and without awakenings. Sleep. 2019;42(11). ↩︎
- Hall MH, Kline CE, Nowakowski S. Insomnia and sleep apnea in midlife women: prevalence and consequences to health and functioning. F1000Prime Rep. 2015;7:63. ↩︎
- Jehan S, Auguste E, Zizi F, Pandi-Perumal SR, Gupta R, Attarian H, et al. Obstructive sleep apnea: Women’s perspective. J Sleep Med Disord. 2016; 3(6): 1064. ↩︎
- Popovic RM, White DP. Upper airway muscle activity in normal women: influence of hormonal status. J Appl Physiol. 1998;84(3):1055–62. ↩︎
- Seeman MV. Why are women prone to restless legs syndrome? Int J Environ Res Public Health. 2020;17(1):368. ↩︎
- Bosworth HB, Bastian LA, Kuchibhatla MN, Steffens DC, McBride CM, Skinner CS, et al. Depressive symptoms, menopausal status, and climacteric symptoms in women at midlife. Psychosom Med. 2001;63(4):603–8. ↩︎
- Baker FC, Willoughby AR, Sassoon SA, Colrain IM, de Zambotti M. Insomnia in women approaching menopause: Beyond perception. Psychoneuroendocrinology. 2015;60:96–104. ↩︎
- Ciano C, King TS, Wright RR, Perlis M, Sawyer AM. Longitudinal study of insomnia symptoms among women during perimenopause. J Obstet Gynecol Neonatal Nurs. 2017;46(6):804–13. ↩︎
- Guthrie KA, Larson JC, Ensrud KE, Anderson GL, Carpenter JS, Freeman EW, et al. Effects of pharmacologic and nonpharmacologic interventions on insomnia symptoms and self-reported sleep quality in women with hot flashes: A pooled analysis of individual participant data from four MsFLASH trials. Sleep. 2018;41(1). ↩︎
- Baker FC, Lampio L, Saaresranta T, Polo-Kantola P. Sleep and sleep disorders in the menopausal transition. Sleep Med Clin. 2018;13(3):443–56. ↩︎
- Hunter MS. Cognitive behavioral therapy for menopausal symptoms. Climacteric. 2020;1–6. ↩︎
- Sweetman A, Lack L, Catcheside PG, Antic NA, Smith S, Chai-Coetzer CL, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with comorbid insomnia: a randomized clinical trial. Sleep. 2019;42(12). ↩︎
- Sweetman A, Lack L, Lambert S, Gradisar M, Harris J. Does comorbid obstructive sleep apnea impair the effectiveness of cognitive and behavioral therapy for insomnia? Sleep Med. 2017;39:38–46. ↩︎
- Talebi M, Tabatabaye KR, Vahedi E. Application of cognitive-behavioral therapy in obstructive sleep apnea: Comparison of CPAP therapy and CBT on the executive functions of the brain. J Sleep Disord Ther. 2017;06(02). ↩︎
- Song ML, Park KM, Motamedi GK, Cho YW. Cognitive behavioral therapy for insomnia in restless legs syndrome patients. Sleep Med. 2020;74:227–34. ↩︎